Cervical cancer has long been a leading cause of death among women worldwide, but recent data indicates a dramatic decline in mortality rates, thanks to the widespread adoption of the human papillomavirus (HPV) vaccine. This breakthrough vaccine, first introduced in 2006, has had a profound impact on the fight against cervical cancer, a disease that was previously responsible for hundreds of thousands of deaths every year.
Understanding the Link Between HPV and Cervical Cancer
Human papillomavirus (HPV) is a group of more than 200 related viruses, some of which can cause cervical cancer. In fact, nearly all cases of cervical cancer are caused by persistent infections with high-risk strains of HPV. Over 70% of cervical cancers are linked to two high-risk HPV types, 16 and 18.
Infections with HPV are common, but in most cases, the body’s immune system clears the virus naturally. However, in a small percentage of women, the virus persists, leading to changes in the cells of the cervix. Over many years, these cellular changes can progress to cancer. For decades, cervical cancer prevention largely relied on regular screenings like the Pap smear to detect abnormal cells before they developed into cancer. However, screening only helps catch the disease once it has already begun to progress.
The HPV Vaccine: A Game Changer
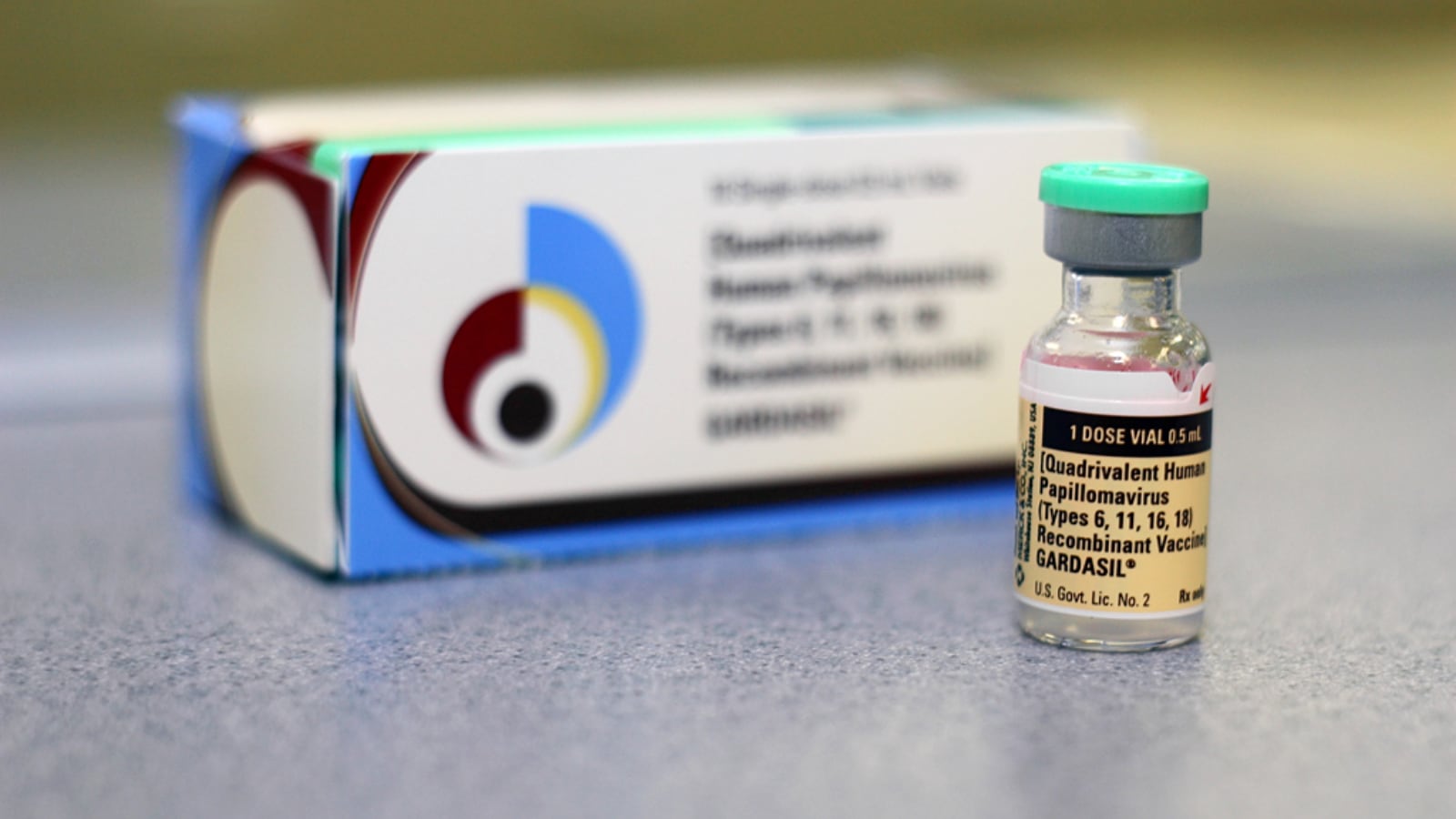
The HPV vaccine, which targets the most common cancer-causing strains of the virus (primarily HPV 16 and 18), provides a proactive method of preventing the infection from ever taking root in the first place. The vaccine has been shown to be highly effective at preventing HPV infections, particularly when administered before individuals become sexually active.
Since its introduction, the vaccine has been offered to young people, primarily girls aged 11 to 12, as part of routine immunization programs in many countries. Some countries have expanded vaccination efforts to include boys, further decreasing the overall burden of HPV-related cancers. Studies have shown that the vaccine dramatically reduces the prevalence of HPV infections, with rates of the targeted HPV strains dropping by up to 90% in vaccinated populations.
Impact on Cervical Cancer Mortality
The most striking impact of the HPV vaccine has been on cervical cancer deaths. In countries where vaccination programs have been widely implemented, there has been a noticeable drop in both the incidence and mortality of cervical cancer.
In countries like Australia, which began HPV vaccination programs in 2007, the decrease in cervical cancer rates has been particularly dramatic. According to recent reports, the introduction of the HPV vaccine has led to a 50% drop in cervical cancer deaths in vaccinated cohorts. Similar declines have been reported in the UK, Sweden, and several other European nations.
The reduction in cervical cancer mortality can be attributed to both the direct effects of the vaccine and its role in enhancing screening programs. With fewer HPV infections leading to precancerous changes, the need for frequent and invasive screening tests has also decreased, easing the burden on healthcare systems and improving quality of life for women.
Global Efforts and Challenges Ahead
While the impact of the HPV vaccine is clear, its full potential is still being realized. Globally, HPV vaccination coverage is uneven. High-income countries, where access to vaccines and healthcare infrastructure is more robust, have seen significant declines in cervical cancer rates. In contrast, many low- and middle-income countries continue to struggle with both access to the vaccine and education around its benefits.
The World Health Organization (WHO) has set an ambitious target to eliminate cervical cancer as a public health problem by 2030. This goal involves vaccinating 90% of girls by the age of 15, ensuring 70% of women receive regular cervical cancer screening by the age of 35, and providing treatment to 90% of women diagnosed with cervical cancer. To meet this target, significant investment in healthcare infrastructure, vaccine distribution, and public awareness will be required, especially in underserved regions.
The Future of Cervical Cancer Prevention
As vaccination rates continue to rise and screening methods become more advanced, cervical cancer is on track to become a rare disease in the future. Advances in HPV vaccine formulations, including vaccines that cover a wider range of cancer-causing HPV types, promise even greater protection. Moreover, the ongoing research into therapeutic HPV vaccines, which aim to treat existing infections and pre-cancerous lesions, could further decrease cervical cancer incidences.
The success of the HPV vaccine represents one of the most significant achievements in public health in recent decades. With continued global commitment and equitable access to the vaccine, the dream of a world where cervical cancer no longer causes preventable deaths is becoming a reality.
By continuing to push forward in vaccination, education, and early detection, the battle against cervical cancer is moving towards a hopeful and transformative future.
Leave a comment